Overview
Heart surgery and how to prepare
This information is dedicated to helping you prepare for your upcoming heart surgery. We understand that facing surgery can be a daunting experience, filled with questions and uncertainties. Our goal is to provide you with the information you need to feel at ease, confident, and well-prepared.
The date of your surgery depends on how urgent the consultant feels your operation is and what tests and examinations you may need before the surgery. When everything is agreed, the admissions co-ordinator will contact you with a planned admission date. You can use this time to prepare. On this page, you'll find practical information about:
- types of heart surgery
- risks and complications
- pre-assessment appointment
- medicines
- hospital bag checklist
While you wait for your surgery date, it's important to use this time to prepare your body, mind, and your home environment. You might want to read the following pages with someone who can support you with getting things ready.
Types of heart surgery
Your doctor will tell you which surgery you are having to treat your condition. They will discuss which type of incision is the best for your condition. In most cases it is a sternotomy.
Sternotomy
An incision around 25cm to 30cm along the sternal bone.
Hemisternotomy
An incision around 10cm to 15cm along the sternal bone.
Right anterior thoracotomy (RAT)
Used for aortic and mitral valve surgery. A 5cm incision at the level of the third rib on the right hand side of the chest wall.
You can click on the relevant box for more information about your type of surgery.
The heart muscle gets its blood supply from the coronary arteries. Sometimes fatty material (atheroma) builds up in these arteries causing them to narrow and sometimes become blocked. This is called atherosclerosis.
If blood is not easily getting through to the heart it can cause pain or discomfort in the chest and sometimes in the arm, neck, stomach or jaw. This is called angina.
Sometimes a piece of the fatty deposit breaks off and a blood clot forms around it and blocks the artery. The heart becomes starved of blood and oxygen and causes a heart attack.
Heart bypass surgery is an operation where a graft is used to get around the narrow or blocked section of the coronary artery. This is called a bypass.
Your doctor will discuss the best treatment option with you. This could also include:
- medicines to manage, control and reduce your symptoms
- angioplasty, a procedure to widen coronary arteries
Using a graft for bypass surgery
Surgeons can use veins or arteries from your chest, leg or arm to help your blood go around the blockage. This is called a coronary artery bypass graft (CABG) operation. These veins or arteries can be safely removed and do not harm your body and health.
They are used as a graft and are attached to the coronary artery to go around (bypass) the blockage. If there is a blockage in more than 1 coronary artery, then you may need a double bypass (2 grafts), or a triple (3 grafts) or quadruple (4 grafts) bypass.
A CABG operation can:
- reduce the risk of further heart attacks
- improve the function of the heart muscle
- stop further episodes of angina
The CABG operation will happen at the same time as your main heart surgery.
Chest arteries are the most common bypass grafts, as they have the best long-term results and can be accessed through the main incision for the cardiac surgery.
Arm arteries are taken from the lower part of the arm. Tests will be carried before and during surgery to make sure that these arteries are suitable for the graft. There are usually no side effects although you may experience some numbness after surgery which is unlikely to last long-term. We may not use these arteries if you have conditions such as Raynaud’s syndrome, carpal tunnel syndrome or painful fingers in cold air.
Veins from the leg may be removed using:
- open vein harvest (OVH) where a single cut is made from the ankle to the knee or groin, depending on the length of vein that is required
- endoscopic vein harvest (EVH) where the vein is removed through a number of small cuts along the leg.
The surgeon will decide which technique to use at the time of your operation.
There are 4 valves in the heart that makes sure that the blood flows continuously around the body in the right direction.
If these valves are damaged or diseased, they may not open properly and obstruct the blood flow (valve stenosis). If they do not close properly blood leaks backwards (regurgitation or incompetence). Both put a strain on your heart. There may not be any symptoms or you may notice increased tiredness, feeling faint or breathlessness.
The 2 values that are usually affected are called:
- Aortic valve. This valve can generally be replaced
- Mitral valve. This valve can sometimes be repaired rather than replaced
If a repair is not possible and a replacement is required, you will receive an artificial heart valve. This will either be made of mechanical parts or of natural tissue.
Mechanical valve
An advantage of having a mechanical valve is that they are more hard wearing than tissue valves. It means that you won’t need to have further surgery in the future. You may initially be aware of your valve making a quiet ticking noise similar to the sound of a ticking watch, especially when the surrounding environment is quiet.
The disadvantage of having a mechanical valve is that you will have to be on a medicine called Warfarin for the rest of your life.
Natural tissue valve
These values are usually made of tissue taken from pigs or cows.
At present we know that these valves last about 10 to 15 years depending on your age. If you choose a tissue valve you may need surgery in the future to replace it if it wears out. You do not need to take Warfarin if you have a tissue valve.
ROSS procedure for congenital heart disease
Your own healthy pulmonary valve (pulmonary autograft) is used to replace your damaged aortic valve. A donated human pulmonary valve (pulmonary homograft/allograft) is used to replace your pulmonary valve.
Dental hygiene
It is very important that your teeth and gums are healthy as if they are infected they can cause the new heart valve to also become infected. Make sure that you see a dentist regularly and at least 12 months before your surgery.
After your surgery, you must tell your dentist that you have received treatment, as you may need antibiotics for some dental treatments.
A thick muscular wall called the septum divides the left and right sides of the heart. A defect in the septum (hole in the heart) causes a strain on the heart. This hole is usually diagnosed at birth but sometimes it is not noticed until later. Symptoms are usually breathlessness or tiredness. Sometimes there are no symptoms but a doctor hears a heart murmur.
The heart is made up of 4 chambers, if the hole is in the wall between the left and right chambers at the top of the heart, this is called an atrial septal defect. If the hole is between the left and right chambers at the bottom, this called a ventricular septal defect.
The hole can be repaired by either sewing the edges together or sewing on a patch if the hole is bigger.
An aneurysm is a swelling of a blood vessel caused by a weak spot in the blood vessel wall.
- Aortic aneurysm occurs in the main artery (the aorta) that leaves the heart. It is repaired by replacing it with a graft which is made from woven polyester (Dacron). It is very durable and usually lasts a lifetime.
- Ventricular aneurysm occurs in the scar where the heart attack has occurred. A scar usually forms in the area of the dead muscle in the heart following a heart attack. This piece of dead tissue is usually removed at the same time as the bypass.
Some patients have an enlarged aortic root. To prevent it from getting bigger, a personalised material sleeve is made to wrap around the aorta. This procedure is called personalised external aortic root support (PEARS).
If you have atrial fibrillation your surgeon may discuss also doing another procedure at the same time.
MAZE. This is a procedure to try to correct atrial fibrillation by creating a specific pattern of scar tissue. It blocks abnormal signals but allows normal heartbeat signals to come through.
Pulmonary vein isolation. This procedure attempts to stop the abnormal electrical signals in your heart that cause heart rhythm problems. It is a form of ablation therapy, using hot or cold substances to create scar tissue. The scar tissues disrupts abnormal electrical signals that cause atrial fibrillation.
Left atrial appendage occlusion. The left atrial appendage is plugged with a device with the aim of stopping blood clots from forming.
This procedure does not treat atrial fibrillation but does reduce the risk of having a stroke.
Risks and complications of heart surgery
There are risks and complications with any type of surgery. These are different for each person and can depend on your age, condition and the type of surgery recommended. The consultant will discuss these with you before you agree to have surgery.
We look at the risks of you having surgery and anaesthetic against the risk of you not having a surgery. We will not recommend a procedure if we did not believe the benefits outweigh the risks.
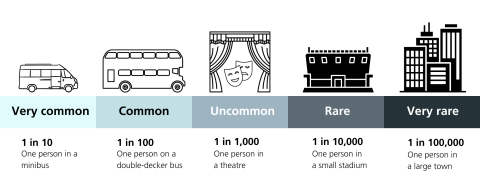
We have designed this chart to help you understand how likely a risk or complication could affect you.
Bleeding
There is a risk of bleeding and some persistent bleeding is normal and expected. Medicine will be used to stop the blood from clotting and the surgeon will stop as much bleeding as possible before the chest is closed. Drainage tubes are placed in the chest so that blood loss can be measured. If bleeding is excessive, it may be necessary to go back to the operating theatre to treat the cause of the bleeding. This usually happens within the first few hours after surgery.
Blood clots
Deep vein thrombosis (DVT) is a blood clot that can develop in the veins of the leg. These may present as a red, painful and swollen leg(s). All surgery carries a risk of DVT. Starting to walk, getting moving and anticoagulant (blood thinning) medicine are the best ways of preventing a DVT.
We will assess your risk of DVT and may give you daily tablets or injections while you are in hospital. If you are at a higher risk of developing a blood clot, we will give you these to take home. If you need daily injections, we will show you or a carer how to administer these or arrange for support at home to do so.
Infection
We will give you antibiotics during your operation to reduce the risk of infection. Despite all precautions, infections can still occur in a small number of patients. Those at increased risk are patients with diabetes, smokers and patients taking medicines such as steroids.
Good personal hygiene is also important to help prevent infection.
The most common sites for infection are:
- Lungs (chest infection). After your surgery you will be given deep breathing exercises to reduce the risk of chest infection.
- Surgical wounds. Surgical sites can become infected because bacteria, both on our bodies and in the environment, can enter the area and cause infection. Serious surgical wound infections may require further surgery or longer term dressing management.
- Bladder
- Heart
Patients who undergo a PEARS procedure (a personalised material sleeve wrapped around the aorta) may develop a fever around day 2 after surgery. This is usually just your body’s response to new material around the aorta but we will test to make sure that it is not an infection. This is very rare (less than 1 in 5000 cases).
Kidney failure
Some people develop temporary kidney problems, called acute kidney injury. This is diagnosed by changes in blood tests and/or not needing to pee (urinate).
It is important that you are well hydrated before your surgery. You will be encouraged to drink water up until 2 hours before your surgery. In severe cases, temporary dialysis (support from an artificial kidney machine) may be required.
Lung injury
Sometimes lungs do not work very well after surgery, particularly in people who have existing chronic lung disease and smokers.
Lung injury affects 1 in 10 people and is treated with special equipment using fitted facemasks in the high dependency unit (HDU), or sometimes with ventilation in the intensive care unit (ICU).
If you do need ventilation, we will keep you sedated. If you need to be on the ventilator for a long time, the breathing tube in the mouth may be changed to a tube going through the front of the neck into the airway, known as a tracheostomy. This will be more comfortable and helps you to recover quicker. The chances of this are 1 in 100 and the tracheostomy can easily be removed when no longer required.
Atrial fibrillation and rhythm problems
About 1 in 4 people may develop a fast, irregular heartbeat (called atrial fibrillation) which is usually treated with medicine.
Symptoms include
- palpitations
- sweating
- feeling sick (nausea)
- dizziness
A few people, particularly those having heart valve surgery, may have problems with a slow heart rate (bradycardia). In most cases, this resolves itself with time however between 1 and 2 in 100 people will need a pacemaker implanted. This is a small procedure that will be performed under local anaesthetic before you leave hospital.
Confusion and delirium
Occasionally patients can feel confused or agitated after surgery which can be distressing for you and your family. This is usually short term and managed with a specialist team. You can read more on our delirium page.
Stroke
Risks of stroke are difficult to predict, however a person’s age, whether you’ve had a stroke before, the type of surgery you are having and whether you have other problems with arteries and veins (peripheral vascular disease) are all contributory factors.
A stroke can occur immediately after surgery and also hours or days later. Most people will make a full recovery but in some cases the effects are long lasting and sometimes fatal.
Death
This is extremely rare and your surgeon will discuss your personal risk with you during your pre-assessment visit and before you sign the consent form.
Paralytic ileus
This is the term that is given to failure of your bowel to work properly. Rarely, it can take several days for your bowels to start working again, causing nausea, bloating and vomiting. In order to treat this, you may be given an intravenous drip and or a tube placed through your nose (NG tube) to drain your stomach.
Allergy
On occasion, patients may develop allergic reactions to drugs that are used during or after surgery. When this is identified, the allergy is treated, and alternative medications are used where possible. Your GP will also be informed of this to update your records locally.
Altered wound-healing
The wound may become red, thickened and painful (forming a keloid scar), this can be more common in Afro-Caribbean people. Massaging the scar with a moisturising cream when it has healed may help.
Pre-assessment appointment
People needing heart surgery will have a pre-assessment appointment. It's very important that you come to this appointment, as this is when we assess your suitability and fitness for surgery and anaesthetic. We do a number of tests to make sure that your heart, lungs and kidneys are working properly.
These tests include.
- an ECG (electrocardiogram)
- a blood test
- a chest X-ray
- an echocardiogram
- swabs for MRSA (Methicillin Resistant Staphylococcus Aureus)
Your doctor or nurse practitioner will explain any further tests you may need. They also give you a physical examination and confirm your full medical history with you.
Medicines
Please bring all of your medicines, including inhalers and eye drops, into hospital with you so we can see exactly which medicines you take.
This also helps prevent delays to your medicine doses in hospital. If you forget, always tell us about any regular medicines you take (including anything you buy over the counter or any herbal or homeopathic medicines) and if you have any allergies to medicines.
Unless you are specifically asked to make changes, please continue to take your medicines as prescribed. Do not make any changes to your usual medicines, or stop taking them, unless you have been advised to do so.
If you have questions about your medicines, please ask a pharmacist or a member of your medical team. Alternatively, you can call our Pharmacy Medicines Helpline on 020 7188 8748 (9am to 5pm).
Medicines that thin your blood
If you are taking any medicines that thin your blood, such as antiplatelet medicines (for example aspirin or clopidogrel) or anticoagulant medicines (for example warfarin or rivaroxaban), please tell your doctor or the nurse as you may need to stop them temporarily before your procedure.
Diabetes
Also tell your doctor or nurse if you have diabetes as you may need to alter the dose of your diabetes medicines, as you will need to fast before the procedure. Further information on stopping any medicines will be given to you when you are given your surgery date. Please ask us if you have any questions.
Hospital bag checklist
When you have a date for your surgery, you can prepare your bag for your stay in hospital. You'll need to bring the following information.
- The name, address, postcode and telephone number for your GP (and also temporary GP if this is required) and your next of kin details.
- A list of all your medicines and times you need to take them (you can bring your latest prescription).
Packing list
- Your admission letter and any information we sent you about your surgery.
- Any medicines including sprays, insulins, patches, creams, drops or inhalers, in their original packaging where possible.
- Small amounts of money (to buy newspapers, television credits or other items).
- Nightclothes and comfortable day clothes.
- Your glasses, contact lenses and any mobility or hearing aids.
- Bathing toiletries and sanitary products; including toothbrush, hairbrush, slippers and dressing gown.
- Items of religious importance to you.
- Something to help occupy your time either when waiting for surgery or on the ward.
- Your mobile phone and charger.
- If you have special dietary requirements you may want to bring a light snack. Please do not bring any food that requires reheating.
- Patients who wear a bra are recommended to wear one after surgery for support. This should not be underwired to avoid pressing on the wound and a front fastening bra is easier to wear. Specially designed bras for post-cardiac surgery can be bought on the high street and online. It is worth wearing before surgery so that you can get used to it.
Resource number: 5454/VER1
Published date: December 2023
Review date: December 2026
