Overview
Awake breast surgery without a general anaesthetic
This information is about having awake breast surgery without a general anaesthetic to make you sleep during the operation.
Most people have a general anaesthetic for breast surgery. We often give the general anaesthetic medicine together with some chest wall nerve blocks. This involves injecting a local anaesthetic medicine into the back and front of your chest to:
- make the nerves numb
- ease the pain after the operation
In some cases, it is possible to have the operation without a general anaesthetic at all. We can use the chest wall nerve blocks by themselves to make the area being treated numb.
The aim of this information is to describe the process of having awake breast surgery. It explains:
- the benefits of awake breast surgery
- the risks of local anaesthetic injections
- how we give you the local anaesthetic injections
- what to expect afterwards
If you have any questions, please speak to the anaesthetic specialist doctor (anaesthetist) or a doctor or nurse caring for you.
Benefits of awake breast surgery
There may be some situations where it is safer for us to do breast surgery when you are awake. This is because we believe that a general anaesthetic would be a high risk to your health.
Examples of when awake breast surgery might be suitable include if you:
- are afraid of having a general anaesthetic or want to avoid this for another reason
- have severe heart or lung disease, which a general anaesthetic might make worse
- are frail
- previously had surgery on your throat or neck and it might be difficult to look after your airway (secure a breathing tube) during a general anaesthetic
Your anaesthetist talks to you in detail about:
- your medical conditions
- the possible risks of having a general anaesthetic
- if awake breast surgery might be a safer and better option for you
Risks of local anaesthetic injections
When you have awake breast surgery and we give you injections of local anaesthetic, your safety is our priority. However, all medical procedures involve some risks.
People can interpret words and numbers in different ways. This scale can help you to understand how likely you are to have a side effect or complication.
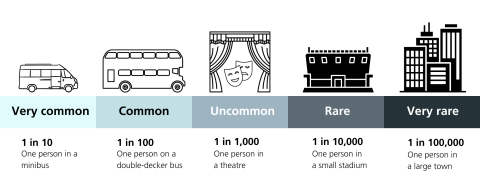
The following table lists the possible risks of local anaesthetic injections and how likely they are to happen.
| Possible risks of local anaesthetic injections | Likelihood of risks happening |
|---|---|
| Bruising at the site of the injections | Very common (1 in 10) |
| Low blood pressure (we can give you medicines to treat this) | Common (1 in 100) |
| Temporary drooping of the eyelid (called Horner's syndrome) | Common (1 in 100) |
| Bleeding | Rare (1 in 10,000) |
| Damage to the covering of the lung, which can cause the lung to collapse to some extent (called a pneumothorax) | Rare (1 in 10,000) |
| A reaction to the local anaesthetic medicine | Rare (1 in 10,000) |
| Infection | Very rare (1 in 100,000) |
|
Nerve injury causing some numbness or weakness that does not resolve within a few days of your surgery |
Very rare (1 in 100,000) |
Having the local anaesthetic injections
We take you into the room where we plan to give you the local anaesthetic injections. The team looking after you:
- checks your details with you
- attaches some equipment that monitors your heart rate, blood pressure and oxygen levels
- puts a thin plastic tube called a cannula into a vein in your hand or arm
Paravertebral block
The first procedure is called a paravertebral block. We give you a series of local anaesthetic injections in the back next to your spine at the level of your shoulder blades.
We inject local anaesthetic in the back because most nerves that supply your breast come from here. If we target the nerves at this point before they spread out over your chest, we can numb them more effectively.
- We usually do the procedure with you lying on your front. However, you can also lie on your side or sit up for the procedure.
- The anaesthetist may give you some sedative medicine to make you feel more relaxed.
- We clean your skin thoroughly and put some clear jelly on it.
- The anaesthetist uses an ultrasound machine to scan the inside of your back. They can then see where the important structures are and guide the local anaesthetic needle to the correct place.
- Your anaesthetist injects some local anaesthetic into the skin with a small needle to make this area numb first.
- The anaesthetist puts in the needle used for the paravertebral block and injects the local anaesthetic. This may cause some temporary discomfort. At this point, we ask you to take some slow, deep breaths.
- After the injection, your anaesthetist scans up and down your back with the ultrasound machine. They can then check that the local anaesthetic has spread to cover all the areas where the nerves supplying your breast are found.
PECS block
The second procedure is called a PECS block. We give you a couple of local anaesthetic injections into the front and side of your chest.
You need this procedure because a few nerves that supply your breast do not come from your back. This means that we need to make them numb with a separate injection.
The process is similar to a paravertebral block.
- You have the procedure lying on your back.
- We clean your skin thoroughly and put some clear jelly on it.
- Using the ultrasound machine, the anaesthetist positions the needle and local anaesthetic injection into the correct place.
What to expect afterwards
The local anaesthetic injections take about 30 minutes to work.
Your anaesthetist does some checks to make sure that your chest is numb enough for the surgery. We then bring you into the operating room, where the surgical team is waiting for you. They:
- clean your chest thoroughly with an anti-septic solution
- put some sterile cloths on your chest, which block your view of the area being treated
Sometimes, the local anaesthetic does not spread to all the nerves as well as we would like. We may then need to give you extra pain relief, including top-up injections of local anaesthetic.
Please be reassured that if your chest wall nerve blocks do not work well enough, we will not do the surgery. The team will then talk to you about what the next options could be.
Anxiety about being awake for the operation
If you are anxious about being awake for the operation, we can:
- give you sedative medicine to make you feel more relaxed
- play a selection of your favourite music during the operation
Your anaesthetic team is with you throughout the operation. They take good care of you and can deal with any concerns that you may have during the surgery.
Pain relief after the operation
The effects of the local anaesthetic wear off gradually. You should continue to get good pain relief from the local anaesthetic for 24 hours after the operation. We also give you the same painkillers to take home that we would have prescribed if you had a general anaesthetic.
Call 999 or go to A&E now if you have:
- unexplained shortness of breath
- pain that is not well controlled by the painkillers that we have given you

